My journey with battling depression and anxiety has been long, and it recently took an interesting turn nine months ago. I decided to record my story here in case it helps someone else.
I can remember fighting anxiety and depression in grade school, when I was dealing with bullying that involved death threats, rape threats, and sexual assault. I had also survived a home explosion and witnessed the abuse of a close friend. (You can search my blog for more on this.)
All of that is to say, by the time I was 15, I had been through a lot of trauma. I was very blessed to have parents who got me into counseling with a Christian psychologist. After several months of counseling and training in coping strategies, I was put on Zoloft. I noticed a difference about a week in. I’ve been in and out of counseling since, depending on whether I could find a good counselor each time I’ve moved. But I’ve been on Zoloft since.
I gave birth to my first baby when I was 28. The depression and anxiety was serious. I didn’t reach out for help because I thought the depression was mainly due to some really difficult things going on in my life then. The anxiety was also much worse than the depression, and I was unaware that postpartum anxiety is a real thing.
Three years later, I gave birth to my second baby, and my world fell apart. The nurses became alarmed before I even left the hospital. My OB immediately increased my Zoloft to the highest dose. By the time I went home a few days later, all I could do was sit and tremble and cry. I felt like the weight of the world was crushing me. The feeling of dread and dysphoria was so intense that it drowned out everything. I remember we jh ate at Qdoba, and I just sat at our table and cried. In public. I couldn’t stop shaking. I was trembling uncontrollably. I was so nauseous I gagged every time I tried to eat. I loved my new baby, and I loved my husband and toddler. I forced myself to hold and nurse my baby because I knew that’s what Normal Me would do, but that’s about all I could handle.
We had a consultation with an integrative pediatrician who specializes in oral ties and is also a licensed breastfeeding consultant. We went to have my baby checked for tongue and lip ties. I remember the doctor saying, “Your baby is fine! But you’re not. Your postpartum anxiety and depression is very severe.” The doctor explained that the same thing happened to her with her fourth child. She said that progesterone (a hormone) is very high during pregnancy, but then it drops quickly after childbirth. For some women, it plummets so low and so quickly that they go into progesterone withdrawal. I was in withdrawal. The shaking and the nausea made so much sense now.
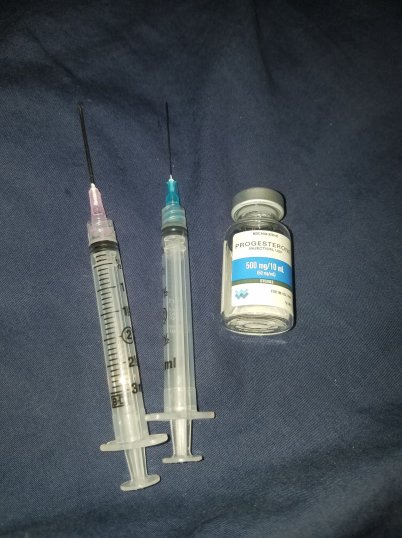
The doctor prescribed me progesterone injections, which consisted of sesame oil, progesterone from yams, and benzyl alcohol. The nurse gave me one injection while instructing my husband, and my husband gave me the second injection. I had about seven more injections to do, one injection every other day. My husband did these for me at home. I remember riding home in the car, those first two doses kicking in, and I felt like I could breathe. I felt like my lungs were no longer crushed. I even felt like eating by the time the two hour car ride was done.
By the end of the course, I felt so much better that it took me several months to realize that there is a difference between “better” and “good.” I was better, but I wasn’t at a good level yet. When my son was 7 months old, I realized I was surviving, but I wasn’t thriving. My kids deserve to have a mom who is thriving. So I made an appointment with my family doctor. We discussed my Zoloft dose, and in that conversation, my doctor was a little alarmed I had been on Zoloft for 16 years. She said the risk of serious side effects increases with time, including heart attack. My mom’s side of the family has a fairly strong history of heart disease, so I was concerned. My doctor also explained that since I had been on Zoloft for so long, it was extremely likely that my body had developed a tolerance to it, causing the Zoloft to be ineffective. I was on 100mg. We decided to wean down to 50mg and check back in two months.
I went through some symptoms that are similar to withdrawal but are officially termed discontinuation syndrome. I was very nauseous, dizzy, irritable, and experienced strong sensory overload, especially with sound. This lasted about a week. But after that, I didn’t feel any different. I felt no more depressed or anxious than I had been. So I went back to my doctor, reported it, and then decreased down to 25mg. Once again, I had the same discontinuation symptoms for a week, but then no change.
It was around this time that I also started incorporating magnesium glycinate. I was taking two capsules of the Nested Naturals brand. The magnesium had quite a noticeable effect on my anxiety. If taking magnesium orally for anxiety, glycinate is the best form and does not have a laxative effect.
On August 21, 2019 I took my last dose of Zoloft. The discontinuation symptoms were pretty rough this time, but I was honestly waiting for much worse. I was waiting to have panic attacks where all I could do was lie on the floor and hyperventilate like when I was a teenager before Zoloft. But that never happened.
I checked back in with my doctor. I was ecstatic that I was doing so well off of Zoloft. I felt no worse. But I didn’t feel any better either, and I wanted to feel better. My energy was lacking, and it needed to improve. I still didn’t have the motivation to do hobbies like I did before my second child was born. I felt very strongly that the problem I was facing was hormone related. I remembered how my lack of energy and motivation began the day I gave birth. I felt that the brain fog and memory issues were more than just “mom brain.” I remembered how effective the progesterone injections were, and I felt strongly that my progesterone was still not right. I asked my doctor if we could test my hormones and see if any were too low or high. She said that hormones could not be my problem, that it would be a waste of time to test them, and that I’d have to ask my OB anyways. She offered to write me a prescription for an antidepressant I hadn’t tried yet. But I wanted something to help me with the root of my problem. I didn’t want something to treat the symptoms. And I wanted something without risk of side effects, if possible.
It just so happened that around this time, a clinic opened up in the city near me that practices functional medicine. I was impressed that the doctors’ goals are to find the problem, and they were willing to do testing to discover what the problem is.
At my consultation, we talked about my history of anxiety and depression, and we decided it was very likely something was off concerning my hormones. Unfortunately, the clinic does not accept insurance, so I had to save up for the hormone test. While I saved up, my energy dropped dramatically. During October and November, I barely had the energy to be a functioning mother. I got my kids clothed, cleaned, and fed every day, but doing more than that was extremely difficult. I was usually in tears by 4 or 5pm, and making dinner seemed like an impossible feat. This felt different than depression; it felt like a physical exhaustion. These months were very difficult for me and for my family.
I did the DUTCH Hormone test in October, and I had another appointment with my nurse practitioner to discuss the results in November. I walked into the appointment thinking I’d be told the same old, “Everything’s normal; we don’t know what’s wrong.” Instead, my NP said, “We have a lot to cover. We got some answers.”
TEST RESULTS
My estrogen (estradiol) was a little below normal. Just as I suspected, my progesterone was low. In fact, it wasn’t just in the low end of normal or a little below normal; my progesterone had gotten to the postmenopausal range. I am only 31 years old. Progesterone should be between 6.0 and 20.0. Mine was at 1.8.

My adrenal hormones were also low. Cortisol is the “stress hormone”. Too much is obviously bad. Too little means you don’t have the proper amount of energy. This is why I was struggling to accomplish goals, to enjoy hobbies. This is why I felt lost in fog. In the chart, the red line should be between the low and high ranges, peaking in the morning. My cortisol (the red line) never peaked; it just consistently dropped. This is why I felt like death by the end of each day.

The results also showed that my body is making some hormones, but then my body fails to convert those into useful forms. For instance, my DHEA levels are good. But my body is failing to convert it into the useful form of DHEA-S in the adrenal glands. This is another reason my energy is gone.
My results also showed that my body has a good amount of methylation activity. (Methylation is a way the body detoxes the daily toxins we encounter.) Despite this activity, methylation is not happening. Some substances are not being detoxed. Other substances that should be converted into something useful are not being converted (like the DHEA). My glutathione (an antioxidant that helps detox) is low. This could be because I have an MTHFR gene mutation, or it could be due to inflammation, or both. Eventually, I plan to have an MTHFR test done.
You know what did not have abnormal levels? Dopamine. And the results for the neurotransmitters showed that my serotonin is likely normal. Zoloft is an SSRI that targets serotonin. My test results essentially show that Zoloft – or any SSRI – would not help me. This explains why I didn’t feel any worse when I got off Zoloft. It is possible, however, that the extreme lack of energy I felt in October and November could be related to stopping Zoloft, which does increase energy. (This is why Zoloft has a black box warning for suicide – because in some people, it doesn’t treat the depression, but it does give them enough energy to plan and carry out a suicide attempt.)
My NP and I did discuss my use of Zoloft. Back when I was a teenager, the Zoloft probably did have a positive effect. I don’t regret using it. I truly had been through so much trauma that I needed both counseling and medication. Antidepressants and medications have their place. However, I was at the point where I felt this was no longer the right answer for my body.
I did feel overwhelmed with these results at first. I wasn’t expecting so many things to be in abnormal ranges. I then felt a lot of anger and sadness that I had been made to feel so foolish for asking my old doc for a hormone test, that I had been so brushed off and dismissed. But I also felt relief that I had found a nurse practitioner who listened to me, who fought for me, who was willing to pore over pages and pages of test results, meet with a team of doctors to discuss healing, and spend so much time explaining all this to me.
My NP and I discussed the gameplan. These hormones are too low, which is due to inflammation, but we still hadn’t discovered the cause of the inflammation. The goal is to learn the cause. Possibilities included a chronic infection or food sensitivities. The test for the chronic infection was very affordable, so I did that one right away. It came back clear. This leaves us with food sensitivities.
The food sensitivity test is over $300, so I am once again saving up. My goal is to have that done by February 2020. Once I know what foods I need to cut out, the inflammation levels will drop, and my body will start regulating hormones the way it should.
For now, my levels are so low that my body needs help getting them back up. I need to function, and I need to be there for my kids. I need to do more than survive. My NP discussed my results with other doctors and also considered some special needs, such as the fact I am breastfeeding. We can’t do anything too potent, and we can’t do any strong detoxes. (Strong detoxes while breastfeeding can dump toxins into the breastmilk.) My NP and her team recommended four supplements to help me. Pregnenolone will help raise my hormones in such a way that cancer is not a concern. I am also taking DHEA to help give my body a boost since I’m not converting that well on my own. I am taking Methyl Renew, to help support my body’s methylation function. This supplement is mainly B vitamins. Lastly, I am taking glutathione, since those levels were low. That will also help me detoxify correctly. I won’t need to be on these supplements forever. This is to get me back on my feet.
I’ve been on the supplements about 2 months now, and I am finally noticing a difference. I’ve organized my kids’ closets. I’ve completely reorganized our storage room and dropped things off for donation. I’ve caught up on things that have been on my to-do list for months. I still have bad days, especially since it is gloomy winter, but I’m doing better than I was a year ago.
My point in sharing all of this is this: If you feel you are struggling with depression or anxiety, and if you feel like medication is not the right answer for your situation, find a doctor who will help you. You might have to look around, and you’d probably have to look into functional, integrative, or holistic doctors, but there are answers out there. If you are a woman who is struggling with depression, anxiety, or extreme brain fog and lack of energy after childbirth, please consider having your hormones checked. You may not have much support in the journey. Our culture is used to prescriptions that act like bandaids. Finding the root cause is hard, and tests aren’t cheap. Yet, I have no regrets.
Last week was my first Christmas without Zoloft in 16 years. It’s the best Christmas I have had in several years. No sudden bouts of weeping. I truly enjoyed celebrating Jesus’ birthday with my family. Today, something in our oven caught fire, and I had to put it out. This is a HUGE trigger that is guaranteed to cause a panic attack and flash back of the home explosion I survived as a child. No flash back. I extinguished the fire, then comforted my daughter, and we moved on with our day together.
I’m getting better!